
There are five cost levers employers can explore right now to offer employees improved benefits, while also keeping costs in check.
The cost of healthcare in the United States has a reputation for being expensive, and deservedly so. According to a study by the Peterson and Kaiser Foundations, the United States spent more than $3.8 trillion on healthcare in 2019, and it will soon top $4 trillion. Employers feel that they’re held captive to annually escalating health plan benefit costs, and employees see their share of premiums and out of pocket costs continue to increase at a higher pace than inflation and their paycheck.
Faced with this reality, as well as a future that promises even higher healthcare costs, current and prospective employees will value companies that have their health-related interests in mind. This is especially true following 2020 and the lingering impact of the coronavirus pandemic. Having an attractive health plan could mean the difference between retaining or losing top talent.
We’re here to report that it’s not all doom and gloom. Employers can offer great, and even improved, health plan benefits to their employees often at reduced costs by breaking out of the box defined by traditional health plans. The trick is finding solutions that provide flexibility. Here are five cost levers employers can explore right now to offer employees improved benefits, while also keeping costs in check.
1. Self-funding
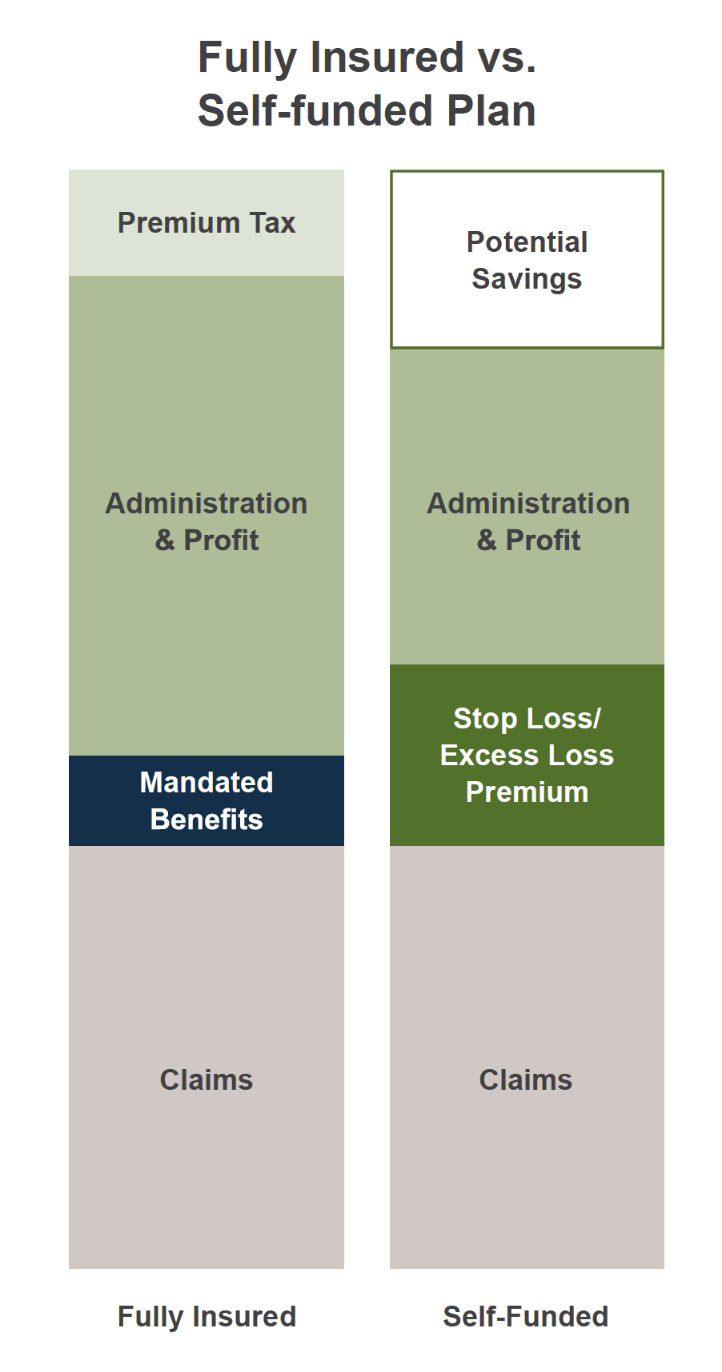
Self-funding is a huge opportunity to control costs while improving care. Through an insurance provider, an employer signs up for a fixed plan and pays a monthly premium, whether claims occur or not. If the plan members don’t use the healthcare they paid for, the insurance company stands to profit. And that they definitely do. Anthem Inc.’s reported net income for 2020 was $551 Million. Another barrier employers face in controlling healthcare spend is lack of access to utilization information and data that identifies trends. This is especially true for employers with fully insured plans and less than 100 employees enrolled. These groups typically aren’t given access to data that could be used to improve the plan experience for members, and to justify or refute escalating premium increases.
A self-funded plan allows an employer to create a customized plan that serves its employees and company well as they take control of quality and cost. With an independent Third Party Administrator (TPA) partner providing administration and guidance, self funded plans often see less administration cost than equivalent fully insured plans. The savings realized in administration can be used to fund stop-loss insurance, which offers less risk and higher reward. Stop-loss activates if claims exceed projections, but if claims are lower than projected, that money can go back into the plan, the employees or the company. Self-funded plans also give the employer access to their data and metrics, allowing them to properly budget for potential future claims and add additional programs or improvements that can both increase employee satisfaction and provide additional cost control. Employers of any size can use a self-funded plan and reap the benefits.
2. Pharmacy and Specialty Drug Strategies
Similar to self-funding, there are a variety of strategies that can be used to control the escalating cost of prescription and specialty drugs. An independent prescription risk management company can be brought in to assess and manage pharmacy and specialty drug needs of employees, providing specialized expertise and solutions that increase value versus expense, make sure costs are in line with norms, and improve user experience and outcomes. Specialty Drug programs can take it a step further by seeking alternative funding for these expensive drugs, making it easy for both employers and employees to save.
3. Virtual Health/Telemedicine Strategies
During the pandemic, many people adapted to virtual applications as an alternative to in-office care and gained confidence in this method of service delivery, whether online or by phone. Employers and employees can save time and money using a telehealth service for a wide range of needs including in-demand behavioral health programs. Telemedicine strategies will continue to evolve to better serve the needs of a growing online population and are an easy way to improve healthcare access for employees at a lesser cost.
4. Population Health
Knowing your employees and their potential health risks can give employers an advantage in keeping health costs low. Using predictive modeling, population health management can use metrics, such as hospital and emergency department utilization risk scores, or medical and pharmacy claims, to identify at-risk individuals and intervene or coach them to better outcomes. Once identified, at-risk employees can work with professionals that help them navigate their care and work to improve their health and outcomes. Healthier employees translate to fewer catastrophic hospital and emergency room visits, and lower costs for employees and employers alike. The right TPA partner will have solutions in place to help you manage the health of your employee population.

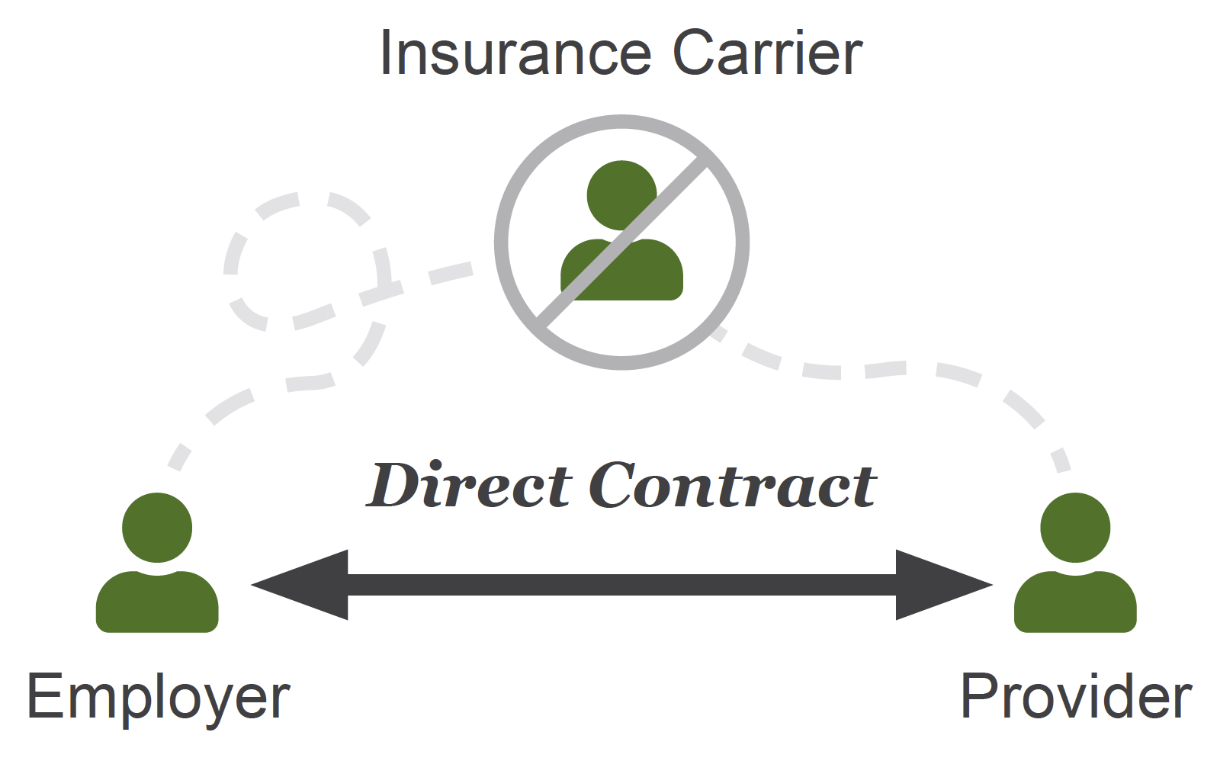
5. Direct Contracting/Direct Primary Care
Direct contracts are growing in popularity and with good reason – they provide another avenue to keep healthcare costs in check because they, in effect, cut out the middleman. Direct contracts based on a Reference-Based Pricing (RBP) reimbursement method can also be used to more accurately predict healthcare costs, with improved forecasting of resource needs and cash flow.
While seeming to offer discounts, fully insured plans through large insurance carrier PPO networks continuously end up costing employers and employees more money than alternative plans. During the negotiation process between providers and insurance carriers, providers will safeguard their revenue by leading with an increased rate that is higher than the actual cost of their services, so they can then discount. Reference-Based Pricing (RBP) plans avoid this pitfall as they don’t rely on a charge master rate. Instead, healthcare through these plans is data-based, with negotiated contracts for service and pharmacy charges that are closer to actual cost. For employees, direct contracts can provide more resources to help them navigate their healthcare, more control over experiences and minimized billing surprises because they have more information upfront. Direct Contracting often results in improved experiences, improved health and reduced costs, a win for both employers and employees.
Conclusion
These five levers are a good foundation for reducing your healthcare costs in 2021, and you don’t have to go it alone. A TPA partner, with their expertise and data, can show you how to reduce your healthcare costs and provide access to a right-sized, self-funded plan for your company, managing all the detail, compliance and employee education and communication.
You can’t keep doing the same thing, especially when it’s not working, and expect different results. Employers can’t continue to bear the brunt of the rising cost of health benefits and shifting that burden to employees isn’t the answer if you want to retain and attract talent. Only 18% of the employers surveyed in Mercer’s National Survey of Employer-Sponsored Health Plans revealed that they will shift more healthcare expenses to employees in 2021. Further, 57% of those surveyed stated they won’t make any changes to reduce costs in their medical plans in 2021. That’s a shame because thinking differently about health benefits in 2021 can affect the health of your company and its employees this year, and for years to come. Talk to your broker today about your options for healthcare coverage.