By L.G. Hanzel Principal & Vice President, RxResults
The universe of drugs that can be considered wasteful is currently estimated to contain more than 800 drugs.*
A guidebook developed in conjunction with the Johns Hopkins Drug Access and Affordability Initiative, “provides information to plan sponsors encouraging them to identify and remove wasteful drugs from prescription drug formularies.” The guidebook noted… Both Branded and Generic Drugs Can Be Wasteful. There is a financial incentive for PBMs to prefer drugs with high prices and large rebates or large spreads, which often results in having wasteful drugs on the formulary.
It’s time to address the misaligned incentives in the formulary and preferred drug list. *Source: Removing Waste from Drug Formularies Guidebook
When setting up an employer’s formulary document and choosing which drugs to cover in the plan, the PBM may, at times, be influenced by their relationship with pharmaceutical companies or their own revenue model.
Your expense is their revenue
Employers need to remember, in a traditional PBM model, the plan’s expense is the PBM and the Pharmaceutical company’s revenue. Employers and their benefit consultants have to ask…is the PBM’s preferred drug list really the employer’s preferred drug list as well?
Leveling the playing field
Pharmacy risk management is changing the benefits landscape. A pharmacy risk manager doesn’t replace a PBM. It serves to enhance a PBM model as an advocate for the plan sponsor and its plan participants.
Driven by the plan sponsor claims data, a pharmacy risk manager leverages informatics, clinical expertise and business processes to formulate actionable insights. And, then implements and executes initiatives that proactively manage pharmacy spend. An evidence-based risk management strategy utilizes reference-based pricing, drug exclusions, prior authorizations and other initiatives.
Evidence-based pharmacy risk management directly meets the challenge of ensuring access to medications proven safe and effective while providing cost control. Results matter…
A 24-month employer group case study leveraging evidence-based research for more than 2,000 drugs across 60-70 classes and sub-classes of drugs yielded significant results in the targeted drug classes.
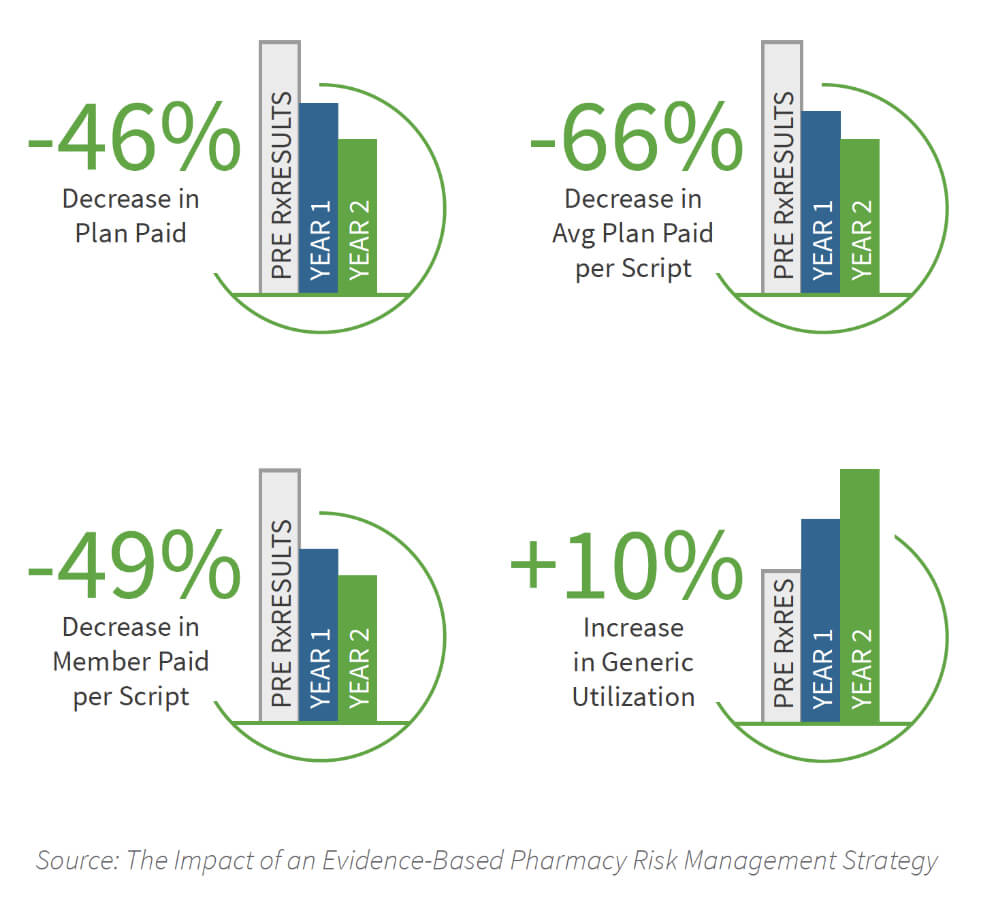
- Plan spend was reduced by 46%
- Member paid per prescription was reduced by 49%
- Plan paid per prescription was reduced by 66%
- Generic utilization increased by 10%
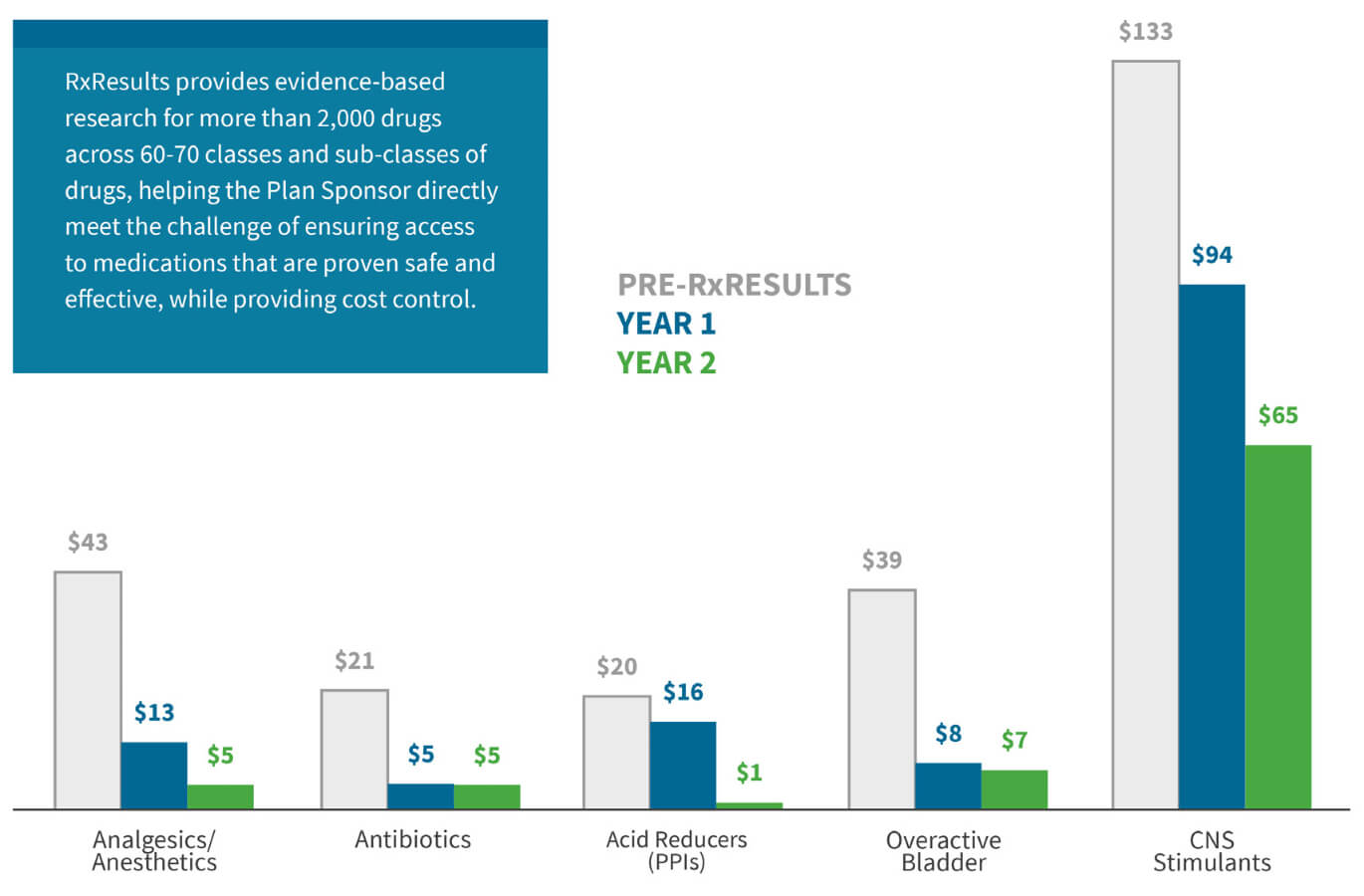
Evidence-based pharmacy risk management significantly reduces Average Plan Paid per Prescription in a sample set of targeted drug classes.
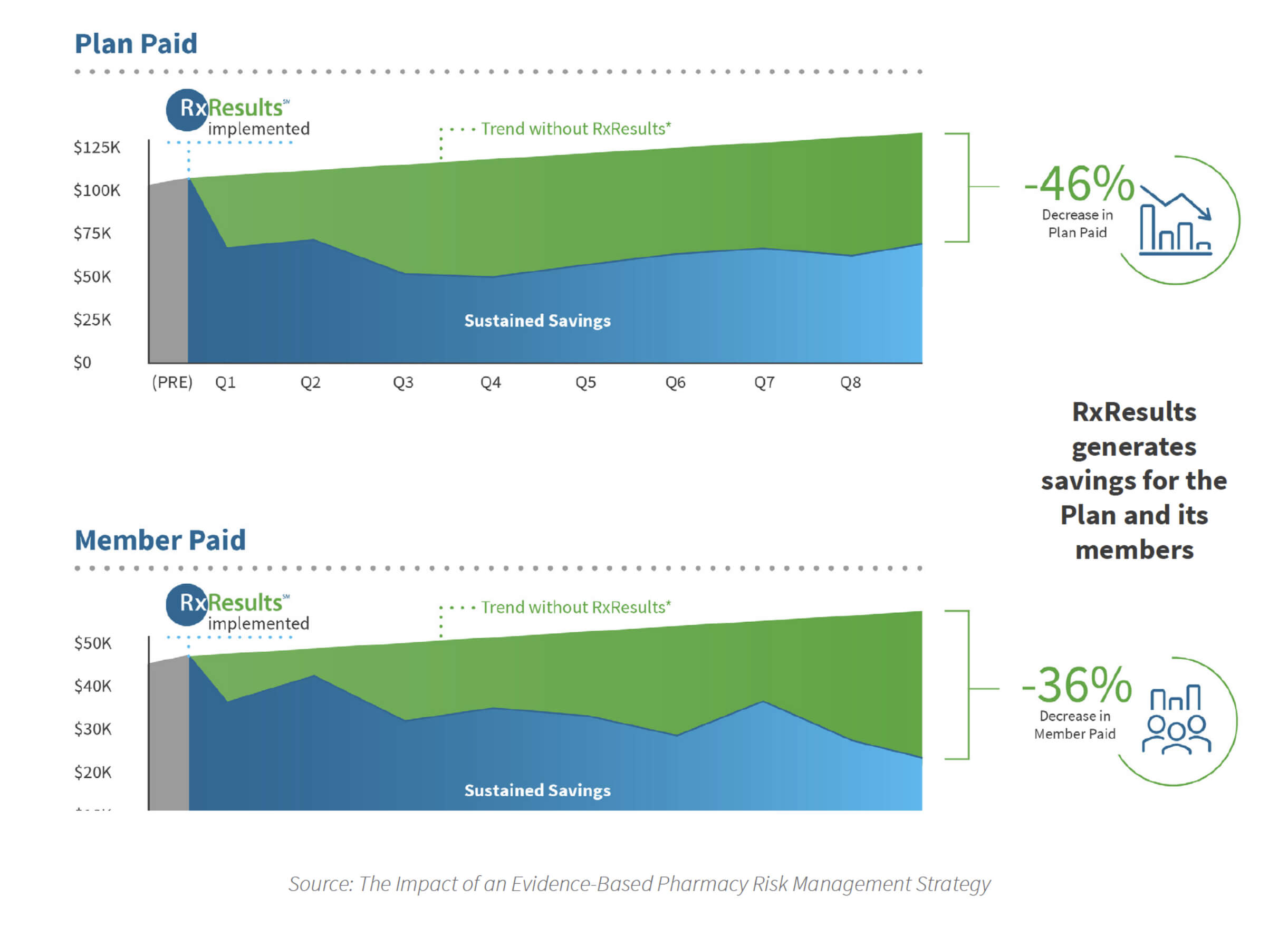
Savings for the Plan and its members.
The Removing Waste From Drug Formularies Guidebook went on to advise…“Given the need to evaluate the clinical value of drugs, and given the very complicated pricing structure within the pharmaceutical supply chain, it is likely that specialized, independent consultants will be required. It is important to have non-conflicted independent consultants to assure objectivity and alignment with the plan sponsor. Health plans, PBMs, and the consultants that represent drug collaboratives or that offer shared savings arrangements may be influenced by the misaligned incentives and revenue streams that contribute to having wasteful drugs on the formularies.”
The employers’ formulary for success is an evidence-based preferred drug list. Traditional pharmacy benefit management is not enough. Employers and their benefit consultants have to start actively managing their pharmacy risk.
Evidence-based pharmacy risk management directly meets the challenge of ensuring access to medications proven safe and effective while providing cost control. It levels the playing field and allows employers to mitigate risk, optimize plan performance and generate savings.
L.G. Hanzel, a pharmacy risk management strategist, has more than 25 years experience in healthcare, benefits, managed care and technology. L.G. has an extensive background in and knowledge of the self-insurance industry and healthcare informatics. L.G. is actively involved in the Self-Insurance Institute of America, Health Care Administrators Association, the National Business Coalition on Health and other regional business health coalitions.
About RxResults: RxResults, a joint-collaborative with the nationally recognized University of Arkansas for Medical Sciences, continuously reviews the latest studies and research on drug outcomes and leverages proprietary informatics, clinical expertise and business processes to identify trends, highlight concerns and formulate actionable insights. RxResults’ core competencies include Specialty Drug Management and Formulary Risk Management.
Click here to connect with LG Hanzel on LinkedIn
Click here to visit the RxResults website
Impact of an Evidence-Based Pharmacy Risk Management Strategy: Download the Case Study Here
Click here to visit the MONEYPILL series LinkedIn page and download other volumes
